How to Identify Your Triggers (Without Reliving the Trauma)
You're having a normal day. Everything's fine. And then something happens, a sound, a smell, a tone of voice, a specific situation, and suddenly you're not fine.
Your heart races. Your chest tightens. You feel panicked, angry, or numb. You want to run, fight, or shut down completely.
And you might not even know why.
This is what a trigger feels like. It's your nervous system reacting to something in the present as if it's a threat from the past. Your body remembers what your mind might have tried to forget.
Triggers are real. They're not "overreactions." They're not something you can just "get over." They're your brain and body trying to protect you from perceived danger based on past trauma.
But here's the challenge: You can't heal what you can't identify. To work through trauma, you need to understand what triggers you. But the idea of identifying triggers can feel scary, like you have to dig through the trauma all over again.
You don't.
There are gentle, safe ways to identify your triggers without retraumatizing yourself. Ways that honor what you've been through while helping you understand your reactions so you can start healing.
Let's talk about what triggers actually are, how to recognize them, and how to identify yours, carefully and safely.
What Are Triggers?
A trigger is anything, an experience, sensation, person, place, or situation, that reminds your nervous system of a past trauma, causing you to react as if the trauma is happening again.
Triggers can be:
External: Something in your environment (a sound, smell, place, person, date on the calendar)
Internal: Something inside you (a thought, emotion, body sensation, memory)
When you're triggered, your body responds with a trauma response:
Fight: Anger, aggression, defensiveness
Flight: Panic, urge to escape, avoidance
Freeze: Numbness, dissociation, shutting down
Fawn: People-pleasing, over-accommodating, losing yourself
These responses are automatic. They're not conscious choices. Your nervous system is reacting to what it perceives as danger, even when you're objectively safe.
Why Triggers Happen: Your Brain Is Trying to Protect You
Here's what's happening in your brain when you're triggered:
During trauma, your brain encodes the experience differently than normal memories. Traumatic memories get stored in fragments, sensory details, emotions, body sensations, without the usual context of time and safety.
So when something in the present resembles something from the trauma, even remotely, your brain says: "Danger! I've seen this before!" And your nervous system activates the same survival response it used during the original trauma.
Your trigger response isn't a flaw. It's your brain trying to protect you. It's saying: "This happened before and it was dangerous. We need to be ready."
The problem is, your brain doesn't always distinguish between actual danger and something that just reminds you of danger. A raised voice might trigger you because it sounds like the yelling during your trauma—even if the person isn't actually threatening you.
Understanding triggers isn't about blaming yourself for your reactions. It's about recognizing the pattern so you can teach your nervous system: "That was then. This is now. I'm safe."
Common Types of Triggers (Across Different Traumas)
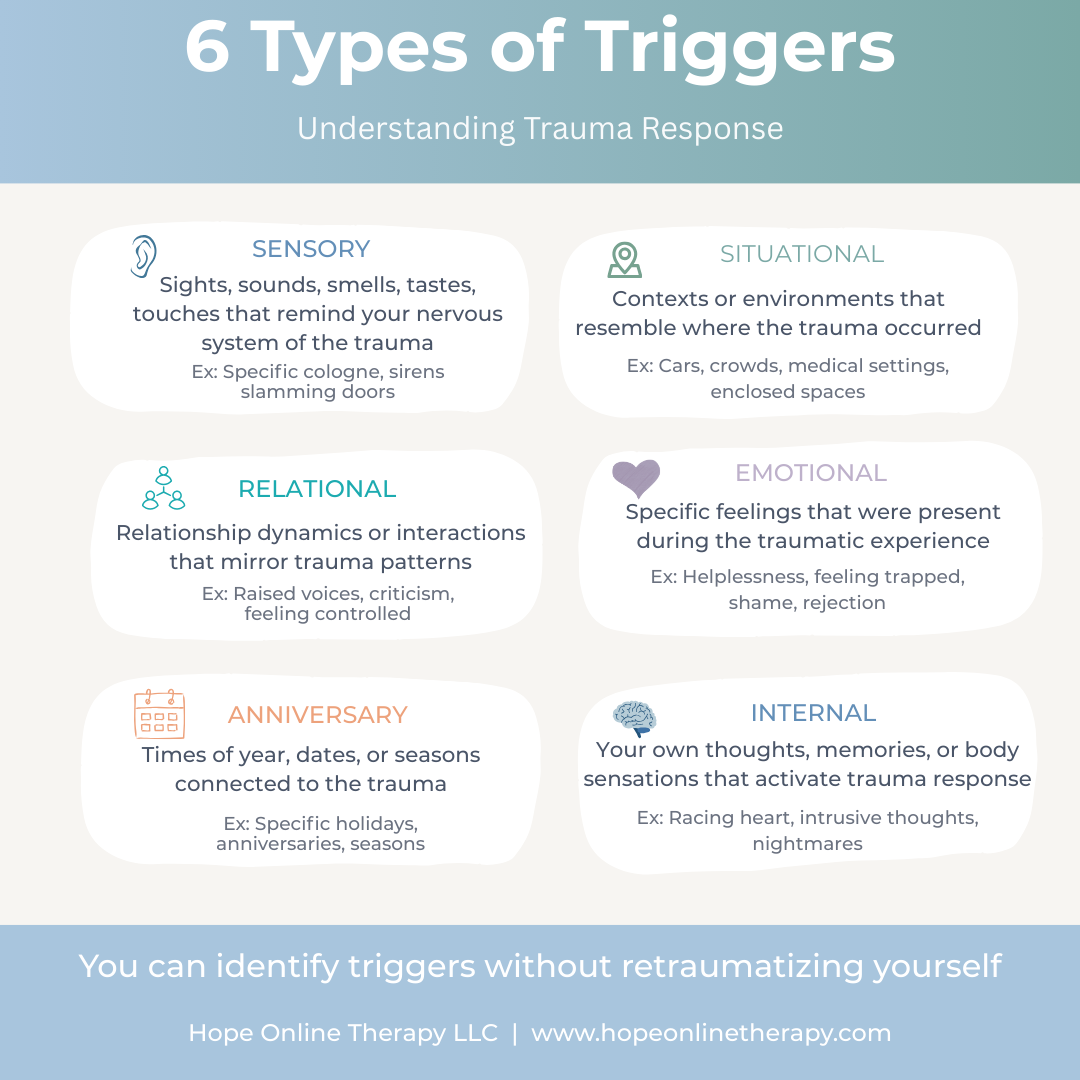
Triggers are unique to each person and their specific trauma. But understanding common categories can help you start recognizing yours.
Sensory Triggers: Your senses are directly linked to memory, a smell, sound, sight, touch, or taste can instantly activate a trauma response. A specific cologne, slamming doors, fireworks, certain foods, or being touched unexpectedly can all trigger reactions based on what was present during your trauma.
Situational Triggers: Contexts that resemble your trauma environment, cars (accident trauma), crowds (assault trauma), medical settings (medical trauma), enclosed spaces (confinement trauma), being alone at night, or conflict situations.
Relational Triggers: Relationship dynamics that mirror trauma patterns, raised voices, criticism, feeling controlled, someone being angry (even if not at you), intimacy, abandonment, or even excessive niceness if your trauma involved manipulation.
Emotional Triggers: Feelings that were present during trauma, helplessness, feeling trapped, shame, rejection, being out of control, or feeling dismissed. These emotions in the present can activate the trauma response even when the situation is objectively safe.
Anniversary Triggers: Times of year, dates, or seasons connected to trauma, the anniversary of the event, specific holidays, seasons, or other significant dates. Your body often remembers even when your mind tries to forget.
Internal Triggers: Your own thoughts, memories, or body sensations, intrusive memories, nightmares, specific physical sensations (racing heart, nausea, tension), or thoughts related to the trauma.
Example: A woman who experienced childhood abuse finds herself panicked when encountering a specific cologne decades later. A combat veteran feels triggered when their heart rate increases during exercise because elevated heart rate was present during combat. Someone avoids social gatherings entirely because the environment triggers memories of assault.
Signs You've Been Triggered (Even If You Don't Realize It)
Sometimes triggers are obvious, you have a panic attack, a flashback, or an intense emotional reaction.
But triggers don't always announce themselves clearly. Sometimes you're triggered and don't even realize it.
Subtle signs you might be triggered:
You suddenly feel irritable, angry, or defensive for "no reason"
You withdraw or shut down emotionally
You become hypervigilant, scanning for danger, unable to relax
You feel disconnected from your body or surroundings (dissociation)
You have an urge to escape the situation or avoid something
Your body feels tense, your breathing becomes shallow, your heart races
You feel an overwhelming need to control the situation or people around you
You become overly compliant or people-pleasing (fawn response)
You can't concentrate or think clearly
You feel suddenly exhausted or drained
The key indicator: Your reaction feels disproportionate to the current situation. You're responding to something your nervous system perceives, not what's actually happening in the present.
How to Identify Your Triggers (Gently and Safely)
You don't need to dissect your trauma to identify your triggers. You can work backward from your reactions.
Here are gentle, trauma-informed ways to start recognizing patterns:
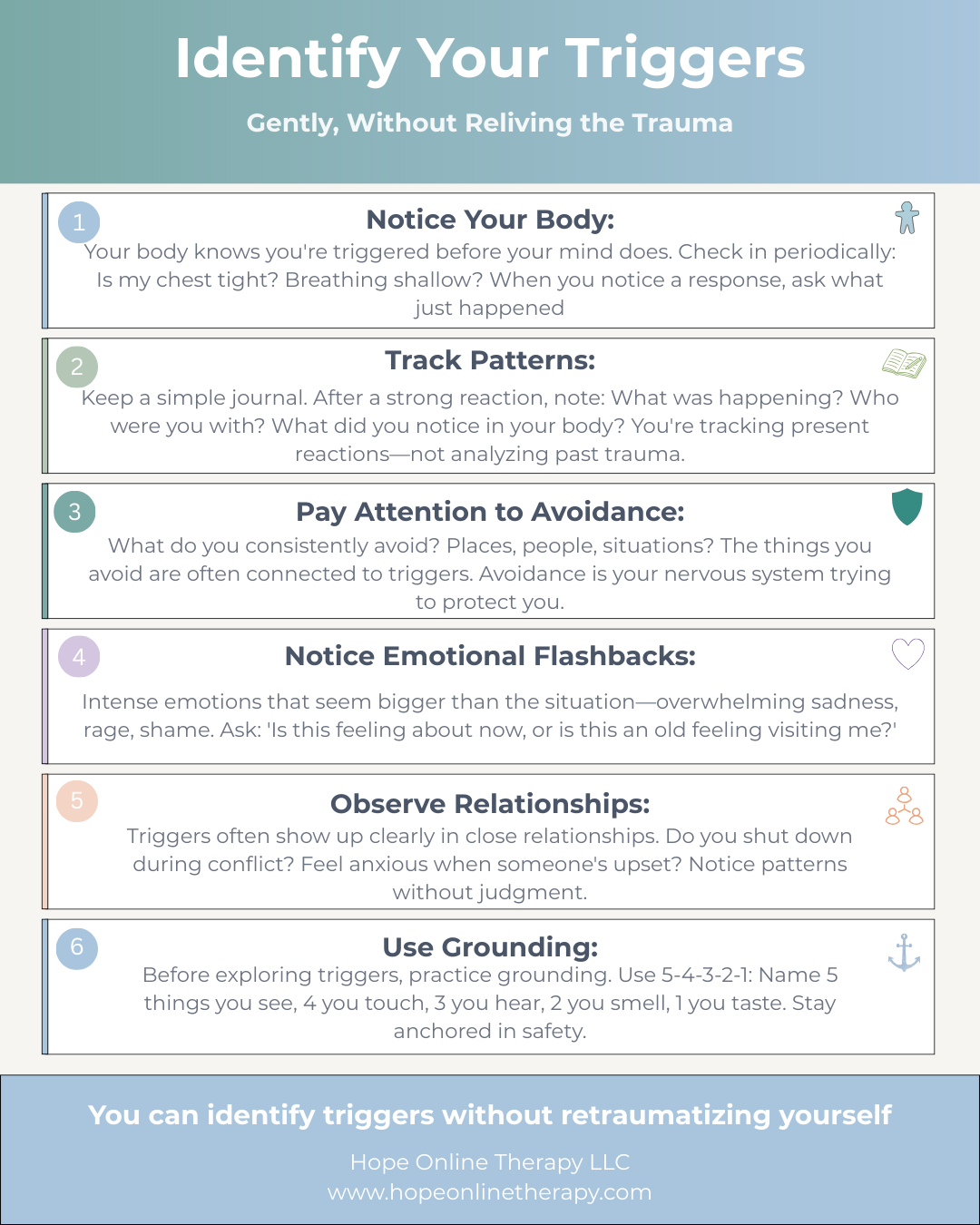
1. Notice Your Body's Responses
Your body often knows you're triggered before your conscious mind does.
How to practice:
Throughout your day, check in with your body periodically
Notice: Is my chest tight? Is my breathing shallow? Are my shoulders tense? Is my stomach upset?
When you notice a physical response, pause and ask: "What just happened? What was I thinking about? What was I doing? Who was I with?"
Why it works: Your body holds the memory of trauma. Physical sensations often precede conscious awareness of being triggered. Learning to notice body signals helps you catch triggers early.
Example: You notice your jaw is clenched and your shoulders are up by your ears. You pause and realize you just got an email from a particular colleague. This might indicate that person or their communication style is a trigger.
2. Track Patterns Without Analyzing the Trauma
You can identify triggers by noticing patterns in your reactions, without diving into the traumatic memory itself.
How to practice:
Keep a simple trigger journal (see template below)
After a strong emotional or physical reaction, note:
What was happening just before?
Where were you?
Who were you with?
What were you doing?
What did you notice in your body?
How did you respond?
Why it works: Over time, patterns emerge. You might notice you always feel anxious in crowded spaces, or you shut down after conflict, or you feel panicked around a certain time of year. You're identifying the trigger without having to explore the original trauma.
Important: You don't need to write about the trauma itself. You're just tracking present-day reactions and looking for commonalities.
3. Pay Attention to Avoidance
What you avoid can reveal your triggers.
How to practice:
Notice what you consistently avoid (places, people, activities, situations)
Ask yourself: "What am I afraid will happen if I do this?"
The thing you're avoiding is likely connected to a trigger
Why it works: Avoidance is a protective response. You're instinctively staying away from things that might trigger you. Recognizing avoidance patterns helps you identify triggers indirectly.
Example: You realize you always decline invitations to go out at night. When you explore why, you recognize that being out after dark makes you feel unsafe—a trigger related to a past trauma that occurred at night.
4. Notice Emotional Flashbacks
Emotional flashbacks feel like intense, seemingly unprovoked emotional states, overwhelming sadness, rage, shame, or fear that feels bigger than the current situation.
How to practice:
When you feel an intense emotion that seems disproportionate, pause
Ask: "Is this feeling about now, or is this an old feeling visiting me?"
Notice if the intensity decreases when you remind yourself: "This is a flashback. I'm safe now."
Why it works: Emotional flashbacks are your body re-experiencing the emotions from the trauma without the conscious memory. Recognizing them as flashbacks helps you identify the emotional triggers without having to fully relive the traumatic event.
Example: Your partner forgets to text you back and you feel overwhelming panic and abandonment—far beyond what the situation warrants. This might be an emotional flashback to earlier experiences of abandonment or neglect.
5. Observe Your Relationships
Triggers often show up most clearly in close relationships.
How to practice:
Notice patterns in your relationships
Do you tend to shut down during conflict?
Do you become anxious when someone is upset, even if it's not at you?
Do you feel triggered by intimacy, vulnerability, or closeness?
Do certain relationship dynamics (being controlled, being ignored, being criticized) consistently provoke strong reactions?
Why it works: Trauma often affects how we relate to others. Relational patterns can reveal underlying triggers without requiring you to analyze the original trauma.
Example: You notice you always pull away when your partner tries to have deep conversations. This might indicate that vulnerability or emotional closeness is a trigger, possibly connected to past experiences where vulnerability wasn't safe.
6. Use Grounding Techniques When Exploring
When you're starting to identify triggers, it's important to stay grounded in the present.
How to practice:
Before exploring triggers, establish a grounding practice
Use the 5-4-3-2-1 technique: Name 5 things you see, 4 you can touch, 3 you hear, 2 you smell, 1 you taste
Keep one foot in the present while observing your reactions
If you start to feel overwhelmed, stop and ground yourself
Why it works: Grounding keeps you anchored in safety while you observe your reactions. It prevents the exploration from becoming retraumatizing.
A Simple Trigger Tracking Template
You don't need anything elaborate. A simple notebook works.
After a strong reaction, jot down:
Date/Time:
What happened (briefly): Example: Was in a crowded grocery store
What I noticed in my body: Example: Heart racing, chest tight, felt like I couldn't breathe
What I felt emotionally: Example: Anxious, panicked, wanted to leave immediately
My response/behavior: Example: Abandoned my cart and left the store
Possible trigger: Example: Crowds? Feeling trapped? Noise level?
After a few weeks of tracking, look for patterns:
Are certain places consistently triggering?
Are specific people or relationship dynamics triggering?
Are particular times of year difficult?
Do specific body sensations show up repeatedly?
The patterns will reveal your triggers, without requiring you to analyze the trauma itself.
What to Do When You Identify a Trigger
Identifying a trigger is the first step. Here's what to do next:
1. Validate yourself. "This is a real response to real trauma. I'm not overreacting."
2. Name it. "I'm being triggered right now. This is my nervous system trying to protect me."
3. Ground yourself. Use grounding techniques to bring yourself back to the present.
4. Create a safety plan. If you know a trigger is coming (like an anniversary date or an unavoidable situation), plan ahead:
How will you support yourself?
Who can you reach out to?
What grounding techniques will you use?
What boundaries do you need?
5. Work with a trauma-informed therapist. A therapist trained in trauma can help you process triggers safely using evidence-based approaches like EMDR (Eye Movement Desensitization and Reprocessing) or trauma-focused CBT.
When Professional Help Is Essential
Identifying triggers on your own is a starting point, but healing from trauma requires professional support.
You should seek therapy if:
Your triggers are significantly impacting your daily life, work, or relationships
You're avoiding so much that your world is getting smaller
You're experiencing flashbacks, nightmares, or intrusive memories
You're using substances to cope with triggers
You feel unsafe or have thoughts of self-harm
You've experienced complex or severe trauma
Trauma therapy can help you:
Process traumatic memories safely
Reduce the intensity of your triggers
Learn to regulate your nervous system
Distinguish between past danger and present safety
Reclaim parts of your life that trauma has taken
EMDR: A Powerful Tool for Trauma
EMDR (Eye Movement Desensitization and Reprocessing) is an evidence-based therapy specifically designed to help process traumatic memories and reduce triggers.
How it works:
EMDR helps your brain reprocess traumatic memories so they're stored as "past events" rather than "current threats"
It reduces the emotional charge of triggers
You don't have to talk in detail about the trauma for it to work
(For more on how CBT and other therapies help with trauma responses, see our post on cognitive distortions and CBT)
EMDR is particularly effective for:
PTSD and complex trauma
Reducing the intensity of triggers
Processing memories that feel "stuck"
Helping your nervous system recognize safety
A trained EMDR therapist can guide you through this process safely, at a pace that works for you.
You Don't Have to Do This Alone
Identifying triggers can feel vulnerable and overwhelming. And that's okay.
You don't have to figure this out perfectly on your own. Trauma is heavy. It's too much to carry alone. And trying to heal from trauma without support often keeps you stuck in the same patterns.
Working with a trauma-informed therapist means:
You have someone trained to help you identify triggers safely
You're not at risk of retraumatizing yourself
You have tools and techniques designed specifically for trauma
You're learning to regulate your nervous system with professional guidance
You have support when the process gets hard
Healing from trauma is possible. Triggers can lose their power. You can feel safe in your body again.
But it's a journey that's better taken with someone who knows the terrain.
The Goal Isn't to Eliminate All Triggers
Here's an important truth: The goal of identifying and working with triggers isn't to never be triggered again.
The goal is:
To understand your triggers so they're less mysterious and frightening
To develop tools to manage your responses when you are triggered
To reduce the intensity and frequency of your reactions over time
To reclaim parts of your life that trauma has restricted
To feel more in control of your nervous system
Some triggers may always exist. That's okay. Trauma leaves an imprint. But with time, support, and the right tools, those triggers can become less disruptive. They can become something you recognize and manage rather than something that controls you.
You're Not Broken. You're Responding to Trauma.
If you're reading this and recognizing yourself—if you're realizing that your "overreactions," your avoidance, your anxiety, your anger might all be connected to triggers—please hear this:
You're not broken. You're not too much. You're not making it up.
Your nervous system is doing exactly what it was designed to do: protect you. It learned that certain things are dangerous. And it's trying to keep you safe.
The problem is, it's protecting you from ghosts, threats that existed in the past but aren't present now.
Identifying your triggers is the first step toward teaching your nervous system the difference between then and now. Between danger and safety. Between trauma and life.
It's hard work. It's brave work. And you don't have to do it alone.
Need Support Identifying and Healing from Triggers?
If you're struggling with trauma triggers and want professional support, therapy can help.
I work with adults in Texas and Idaho who are healing from trauma—helping you identify triggers safely, process traumatic memories, and reclaim your sense of safety using evidence-based approaches including EMDR and trauma-focused therapy.
Virtual therapy means you can do this important work from a place where you already feel safe—your own home, on your schedule.
Schedule a Free Consultation – Let's talk about how trauma therapy can help you understand your triggers and start healing.
You don't have to keep living in survival mode. Healing is possible, and you deserve support for this journey.
Important Disclaimer
This blog post is for informational and educational purposes only. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
If you are experiencing trauma symptoms, triggers, flashbacks, or mental health concerns, please seek help from a qualified mental health professional. If you are in crisis or experiencing thoughts of self-harm, please contact emergency services or call the 988 Suicide & Crisis Lifeline.
The information provided here is meant to help you understand triggers and begin recognizing patterns, but healing from trauma requires professional support. Always consult with a licensed therapist or mental health provider for personalized guidance.